Our Research
Vouchers 4 Veggies – EatSF, in partnership with the UCSF Action Research Center for Health Equity’s Food Policy, Health, and Hunger research program, conducts research and evaluation measuring the impact of produce prescription and healthy food voucher programs on food security and dietary intake among low-income populations. Through our research we seek to advance nutrition policies that equitably increase healthy food access and improve health. This page highlights our research findings, publications from our founder, Dr. Hilary Seligman, and relevant resources from the field.
UCSF Action Research Center for Health Equity

Our Findings:
Fruit and Vegetable Vouchers in Pregnancy: Preliminary Impact on Diet & Food Security
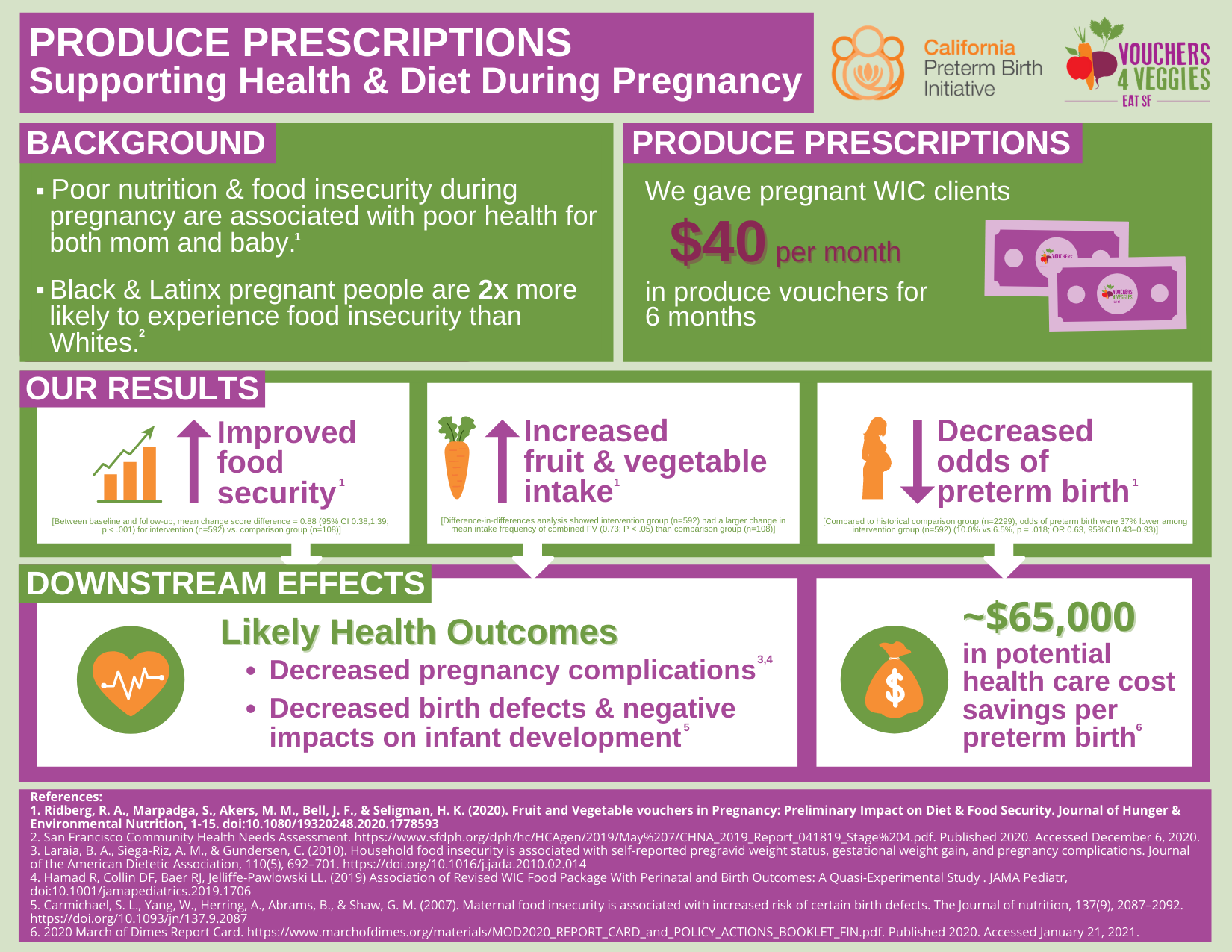
Study Summary:
Pregnancy is a critical time period for supporting food security and maternal nutrition because of long-term potential impacts on the developing fetus. We conducted a pre-/post-analysis of pregnant WIC participants (n = 592) in San Francisco receiving $40/month of fruit and vegetable vouchers in addition to the standard WIC package. We compared pre-/post- changes to a comparison group of non-pregnant WIC participants (n = 108) receiving only the standard WIC package. We observed significant improvements in food security and mean daily frequency of total vegetables, combined fruits and vegetables, salad and non-fried potatoes (p < .05 for all comparisons).
Ronit A. Ridberg , Sanjana Marpadga , Melissa M. Akers , Janice F. Bell & Hilary K. Seligman (2020): Fruit and Vegetable Vouchers in Pregnancy: Preliminary Impact on Diet & Food Security, Journal of Hunger & Environmental Nutrition, DOI:10.1080/19320248.2020.1778593
Effects of Alternative Food Voucher Delivery Strategies on Nutrition Among Low-Income Adults
Study Summary:
Nutrition assistance programs are the subject of ongoing policy debates. Two proposals remain uninformed by existing evidence: whether restricting benefits to allow only fruit and vegetable purchases improves overall dietary intake, and whether more frequent distribution of benefits (weekly versus monthly) induces more fruit and vegetable consumption and less purchasing of calorie-dense foods. In a community-based trial, we randomly assigned participants to receive food vouchers that differed in what foods could be purchased (fruit and vegetables only or any foods) and in distribution schedule (in weekly or monthly installments, holding total monthly value constant). The use of vouchers for fruit and vegetables only did not yield significantly greater improvements than the unrestricted voucher did in terms of fruit and vegetable consumption or Healthy Eating Index (HEI) score. Weekly vouchers also failed to yield significantly greater improvements than monthly vouchers did. Proposed policies to make assistance more restricted or more frequent, while holding benefit value constant, might not improve nutrition among low-income Americans.
Sanjay Basu, Christopher D. Gardner, Justin S. White, Joseph Rigdon, Mandy M. Carroll, Melissa Akers, & Hilary K. Seligman (2019): Effects of Alternative Food Voucher Delivery Strategies on Nutrition Among Low-Income Adults, Health Affairs, DOI: 10.1377/hlthaff.2018.05405
Heterogeneity in the Effects of Food Vouchers on Nutrition Among Low-Income Adults: A Quantile Regression Analysis
Study Summary:
Purpose: To determine whether baseline fruit and vegetable (FV) intake or other predictors are associated with response to food vouchers (change in FV intake) among low-income adults.
Design: Secondary analysis of a randomized, 2 x 2-factorial, community-based trial.
Setting: San Francisco, California.
Intervention: Participants were mailed $20 of food vouchers monthly for 6 months, and randomized to 1 of 4 arms according to: eligible foods (FV only or any foods) and redemption schedule (weekly or monthly).
Results: FV-only weekly vouchers were associated with increased FV intake at the 25th percentile (0.24 cups/day, p ¼ 0.048) and 50th percentile (0.37 cups/day, p ¼ 0.02) of the distribution, but not at lower and higher quantiles. Response to the vouchers diminished 0.10 cups/day for each additional household member (p ¼ 0.02).
Conclusion: Response to food vouchers varied along the FV intake distribution, pointing to some more responsive groups and others potentially needing additional support to increase FV intake. Larger households likely need vouchers of higher dollar value to result in similar changes in dietary intake as that observed in smaller households.
White JS, Vasconcelos G, Harding M, et al. Heterogeneity in the Effects of Food Vouchers on Nutrition Among Low-Income Adults: A Quantile Regression Analysis. American Journal of Health Promotion. September 2020. doi:10.1177/0890117120952991
Relevant Selected Articles from Dr. Hilary Seligman, MD, MAS:
Dr. Hilary Seligman is one of the nation’s foremost experts on the health implications of food insecurity. Dr. Seligman is Core Faculty for UCSF’s Center for Vulnerable Populations at San Francisco General Hospital and Professor of Medicine and of Epidemiology and Biostatistics. She is also the Director of the CDC’s Nutrition and Obesity Policy Research and Evaluation Network, Senior Medical Advisor for Feeding America, and the Director of the Food Policy, Health, & Hunger Program at UCSF.
For more information about Dr. Hilary Seligman, click here.
Please hover and click on the key selected articles from Dr. Hilary Seligman to read more.
Food Insecurity & Chronic Disease
- Food insecurity and hypoglycemia among safety net patients with diabetes
Seligman HK, Jacobs EA, Lopez A, Sarkar U, Tschann J, Fernandez A. Food insecurity and hypoglycemia among safety net patients with diabetes. Arch Intern Med. 2011;171(13):1204-1206. doi:10.1001/archinternmed.2011.287
- Food insecurity and glycemic control among low-income patients with type 2 diabetes
Seligman HK, Jacobs EA, López A, Tschann J, Fernandez A. Food insecurity and glycemic control among low-income patients with type 2 diabetes. Diabetes Care. 2012;35(2):233-238. doi:10.2337/dc11-1627
- Food insecurity is associated with hypoglycemia and poor diabetes self-management in a low-income sample with diabetes
Seligman HK, Davis TC, Schillinger D, Wolf MS. Food insecurity is associated with hypoglycemia and poor diabetes self-management in a low-income sample with diabetes. J Health Care Poor Underserved. 2010;21(4):1227-1233. doi:10.1353/hpu.2010.0921
- Food Insecurity Is Associated with Chronic Disease among Low-Income NHANES Participants
Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants [published correction appears in J Nutr. 2011 Mar;141(3):542]. J Nutr. 2010;140(2):304-310. doi:10.3945/jn.109.112573
- Hunger and Socioeconomic Disparities in Chronic Disease
Seligman HK, Schillinger D. Hunger and socioeconomic disparities in chronic disease. N Engl J Med. 2010;363(1):6-9. doi:10.1056/NEJMp1000072
Food Insecurity & Health Care Expenditures
- Food Insecurity, Healthcare Utilization, and High Cost: A Longitudinal Cohort Study
Berkowitz SA, Seligman HK, Meigs JB, Basu S. Food insecurity, healthcare utilization, and high cost: a longitudinal cohort study. Am J Manag Care. 2018;24(9):399-404.
- Food Insecurity and Health Care Expenditures in the United States, 2011–2013
Berkowitz, S.A., Basu, S., Meigs, J.B. and Seligman, H.K. (2018), Food Insecurity and Health Care Expenditures in the United States, 2011–2013. Health Serv Res, 53: 1600-1620. https://doi.org/10.1111/1475-6773.12730
- State-Level and County-Level Estimates of Health Care Costs Associated with Food Insecurity
Berkowitz SA, Basu S, Gundersen C, Seligman HK. State-Level and County-Level Estimates of Health Care Costs Associated with Food Insecurity. Prev Chronic Dis 2019;16:180549. DOI: http://dx.doi.org/10.5888/pcd16.180549external icon
- Exhaustion of Food Budgets at Month’s End and Hospital Admissions for Hypoglycemia
Seligman HK, Bolger AF, Guzman D, López A, Bibbins-Domingo K. Exhaustion of food budgets at month’s end and hospital admissions for hypoglycemia [published correction appears in Health Aff (Millwood). 2014 Jul;33(7):1304]. Health Aff (Millwood). 2014;33(1):116-123. doi:10.1377/hlthaff.2013.0096
Supplemental Nutrition Assistance Program (SNAP) & Nutrition Incentive Programs
- Cost Effectiveness of Subsidizing Fruit and Vegetable Purchases Through the Supplemental Nutrition Assistance Program
Choi SE, Seligman H, Basu S. Cost Effectiveness of Subsidizing Fruit and Vegetable Purchases Through the Supplemental Nutrition Assistance Program. Am J Prev Med. 2017;52(5):e147-e155. doi:10.1016/j.amepre.2016.12.013
- Supplemental Nutrition Assistance Program (SNAP) Participation and Health Care Expenditures Among Low-Income Adults
Berkowitz SA, Seligman HK, Rigdon J, Meigs JB, Basu S. Supplemental Nutrition Assistance Program (SNAP) Participation and Health Care Expenditures Among Low-Income Adults. JAMA Intern Med. 2017;177(11):1642–1649. doi:10.1001/jamainternmed.2017.4841
- In an unhealthy food system, what role should SNAP play?
Seligman HK, Basu S. In an unhealthy food system, what role should SNAP play?. PLoS Med. 2018;15(10):e1002662. Published 2018 Oct 2. doi:10.1371/journal.pmed.1002662
- Aligning Programs and Policies to Support Food Security and Public Health Goals in the United States
Seligman HK, Berkowitz SA. Aligning Programs and Policies to Support Food Security and Public Health Goals in the United States. Annu Rev Public Health. 2019;40:319-337. doi:10.1146/annurev-publhealth-040218-044132
The following resources and publications highlight and support relevant work around produce prescription (Rx) and nutrition incentive programs. Please hover and click on each resource to read more.
Resources
Food is Medicine Research Action Plan
Nutrition Incentive Hub
- Harvard’s CHLPI
Produce Prescriptions: A U.S. Policy Scan
Mainstreaming Produce Prescriptions: A Policy Strategy Report
- Healthy Food America
Healthy Food Pricing Incentives: Designing Successful Programs
- The Hill
Op-ed: Strengthening WIC to improve health: A prescription for change
- Produce Rx Evaluation & Policy Collaborative
Promising Practices: Implementing a Produce Prescription Program in the Health Care Setting
- Tufts University Friedman School of Nutrition Science and Policy
Infographic: Healthy Food Prescription
Article: Cost-effectiveness of financial incentives for improving diet and health through Medicare and Medicaid: A microsimulation study
Publications
- Healthy Food Prescription Programs and their Impact on Dietary Behavior and Cardiometabolic Risk Factors: A Systematic Review and Meta-Analysis
Saiuj Bhat, Daisy H Coyle, Kathy Trieu, Bruce Neal, Dariush Mozaffarian, Matti Marklund, Jason H Y Wu, Healthy Food Prescription Programs and their Impact on Dietary Behavior and Cardiometabolic Risk Factors: A Systematic Review and Meta-Analysis, Advances in Nutrition, 2021;, nmab039, https://doi.org/10.1093/advances/nmab039
- Effect of a Fruit and Vegetable Prescription Program on Children’s Fruit and Vegetable Consumption
Ridberg RA, Bell JF, Merritt KE, Harris DM, Young HM, Tancredi DJ. Effect of a Fruit and Vegetable Prescription Program on Children’s Fruit and Vegetable Consumption. Prev Chronic Dis 2019;16:180555. DOI: http://dx.doi.org/10.5888/pcd16.180555
- The Impact of the Revised WIC Food Package on Maternal Nutrition During Pregnancy and Postpartum
Hamad R, Batra A, Karasek D, et al. The Impact of the Revised WIC Food Package on Maternal Nutrition During Pregnancy and Postpartum. Am J Epidemiol. 2019;188(8):1493-1502. doi:10.1093/aje/kwz098
- A Pediatric Fruit and Vegetable Prescription Program Increases Food Security in Low-Income Households
Ridberg RA, Bell JF, Merritt KE, Harris DM, Young HM, Tancredi DJ. A Pediatric Fruit and Vegetable Prescription Program Increases Food Security in Low-Income Households. J Nutr Educ Behav. 2019;51(2):224-230.e1. doi:10.1016/j.jneb.2018.08.003
- Diet-Related Medical Expenditure Impacts of a CSA Voucher Program
Rossi, Jairus, and Tim Woods, “Diet-Related Medical Expenditure Impacts of a CSA Voucher Program”, Department of Agricultural Economics Staff Paper No. 497, University of Kentucky, November, 2018.
- The Effects of a Fruit and Vegetable Prescription Program (FVRx)® for Low-Income Individuals on Fruit and Vegetable Intake and Food Purchasing Practices
Slagel, Nicholas & Newman, Taylor & Sanville, Laurel & Dallas, Jackie & Thurman, Sarah & Cummings, Paige & Cotto-Rivera, Edda & Thompson, Jennifer & Lee, Jung. (2018). The Effects of a Fruit and Vegetable Prescription Program (FVRx)® for Low-Income Individuals on Fruit and Vegetable Intake and Food Purchasing Practices. Journal of Nutrition Education and Behavior. 50. S103. 10.1016/j.jneb.2018.04.131.
- Merchant Attitudes Toward a Healthy Food Retailer Incentive Program in a Low-Income San Francisco Neighborhood
McDaniel PA, Minkler M, Juachon L, Thayer R, Estrada J, Falbe J. Merchant Attitudes Toward a Healthy Food Retailer Incentive Program in a Low-Income San Francisco Neighborhood. International Quarterly of Community Health Education. 2018;38(4):207-215. doi:10.1177/0272684X18781788
- Participation in a farmers’ market fruit and vegetable prescription program at a federally qualified health center improves hemoglobin A1C in low income uncontrolled diabetics
Bryce R, Guajardo C, Ilarraza D, et al. Participation in a farmers’ market fruit and vegetable prescription program at a federally qualified health center improves hemoglobin A1C in low income uncontrolled diabetics. Prev Med Rep. 2017;7:176-179. Published 2017 Jun 27. doi:10.1016/j.pmedr.2017.06.006
- Incentivizing fruit and vegetable purchases among participants in the Supplemental Food and Nutrition Program for Women, Infants, and Children
Andreyeva T, Luedicke J. Incentivizing fruit and vegetable purchases among participants in the Special Supplemental Nutrition Program for Women, Infants, and Children. Public Health Nutr. 2015;18(1):33-41. doi:10.1017/S1368980014000512